Not all joint pain are symtoms of arthritis, pain in joints pains leads to presence of Borrelia in blood. Today I would like to bring it to your notice, my experience with this bacteria during my stay in Norway.
A few weeks back I developed severe pain in joints without inflammation soon pain become unbearable, intensity of pain was so much that it became impossible to do day to day work including holding a cup of coffee. Fearing that I would be suffering from Arthritis we decided to diagnose it. One thing I really appreciate about my doctor is her diagnostics skill. It’s excellent. Doctor examined me with lot of questions. And her final question came to me “Were you bitten by any bug? I was not sure so she suggested me to go for Blood test and x ray.
To my surprise my blood samples showed presence of Borrelia not all people are aware of this organism and its effects on human so I take privilege of educating everyone about Borrelia.
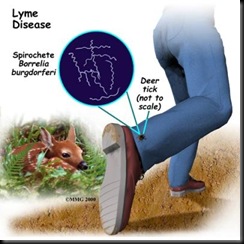
Lyme disease is an infection that derives from a tick bite. The disease has a variety of symptoms, including changes affecting the skin, heart, joints and nervous system. It is also known as Borrelia or Borreliosis.
CAUSES
Lyme disease is caused by an infection from a micro-organism (Borrelia burghdor feri), itself transmitted by a bite from the wood tick, a blood-sucking parasite which normally lives on deer.
Borrelia burgdorferi, is a spirochete. Spirochetes are a group of phylogenetically-distinct bacteria that have a unique mode of motility by means of axial filaments (endoflagella). Spirochetes are widespread in viscous environments and they are found in the intestinal tracts of animals and the oral cavity of humans.
The wood tick is found in many areas, particularly in forests where deer are common. A tick will settle anywhere on a human body, but prefers warm, moist and dark places like the crotch or armpits.
When the tick has found a suitable place on the body, it sticks in its probe to draw up blood, exposing the host to the risk of infection.
SYMPTOMS
Simply seeing a tick somewhere on your body does not mean that you have contracted Lyme disease. Unfortunately, not everyone knows when they have been bitten, so consult your GP if you detect the following symptoms.
- A red spot around the location of the tick's bite. The spot will gradually grow bigger, often with a pale area in the middle. This symptom is called erythema migrans.
- Erythema migrans can also appear at other places on the body where the tick has not bitten. Some people get many red spots.
- Usually one to four weeks will pass between the bite and when erythema migrans appears.
Some patients with Lyme disease feel like they have caught influenza - the symptoms may be:
- drowsiness
- headaches
- mild fever
- joint and muscle pains
- swollen lymph glands.
COMPLICATIONS
Acrodermatitis chronica atrophicans
This is a condition that often develops in older women. Several years may pass from the tick bite until the development of this phenomenon. The symptoms usually involve changes in the skin around the tick bite, such as:
· swelling
· bluish or reddish discoloration of the skin.
Neuro borrelia
About 15 per cent of people with borrelia develop so-called neuro borrelia, between one and five weeks after the tick bite. The central nervous system is affected and the symptoms that result are very mixed and not specific.
- The symptoms often begin with back pain, typically between the shoulder blades and in the neck like a slipped disc. The pain worsens at night.
- Distorted feelings around the area of the bite. The nerves become numb, especially in the face. This may occur at any time up to four weeks after the pain began.
- Sometimes neuro borrelia may present itself as meningitis, with fever, headache and stiffness in the neck.
- In rare cases, the disease may become chronic, with a slowly developing destruction of the nervous system, numbing, partial hearing impairment and the development of dementia.
- Neuro borrelia demands immediate treatment, usually with an admission to hospital.
Inflammation of the joints or Lyme arthritis
This condition may present itself in days or, rarely, years after the bite, but it is very rare. The inflammation of the joints causes pain and swelling. Often, only one joint is inflamed and, rarely, more than three. The most commonly affected joint is the knee followed by the shoulder, elbow, foot, and hip. It has symptoms similar to arthritis.
When treated, the swelling will go away in about one to four weeks but it may return in later months or even years.
DIAGNOSIS
A diagnosis of Lyme disease is more likely if the patient remembers a tick bite and presents the doctor with the erythema migrans rash.
To make a firmer diagnosis the doctor may take a blood sample to determine whether the patient has developed an antibody towards Lyme disease in their blood. Antibodies can typically be found between two and four weeks after contracting the disease, but sometimes the antibodies do not appear for up to eight weeks. This means that the patient may have Lyme disease even though the antibody test is negative. On the other hand, a positive antibody test does not necessarily mean that Borrelia has recently been contracted. The antibodies may be found in the blood several years after an infection is over. Unfortunately, the antibody test is not a very efficient diagnostic tool: false-positive results are common.
If the doctor suspects neuro Borrelia then hospital admission is required for tests on fluids from the spinal canal. This is to determine whether Lyme disease has entered the nervous system.
In cases of chronic neuro borrelia the treatment may include a CT scan of the nervous system.
TREATMENT
- oral doxycillin (except in children), amoxicillin or cephalosporin antibiotics are the usual first choices.
- when antibiotics by injection are being given, then benzylpenicillin, cefotaxime and ceftriaxone are the usual choices.
- no particular choice and method is superior to another - the decision is made by the infectious disease specialist and is dependent on the individual circumstances.
PREVENTION
Removing leaves and clearing brush and tall grass around houses and at the edges of gardens may reduce the numbers of ticks that transmit Lyme disease. Reducing and managing deer populations in geographic areas where Lyme disease occurs may reduce tick abundance.
CDC recommends the following for personal protection from tick bites and Lyme disease:
Avoid tick-infested areas, especially in May, June, and July.
Wear light-colored clothing so that ticks can be spotted more easily. Tuck pant legs into socks or boots and shirt into pants or the area where pants and socks meet so that ticks cannot crawl under clothing.
Spray insect repellent containing DEET on clothes and on exposed skin other than the face, or treat clothes (especially pants, socks, and shoes) with permethrin, which kills ticks on contact.
Wear a hat and a long-sleeved shirt for added protection.
Walk in the center of trails to avoid overhanging grass and brush.
After being outdoors, remove clothing and wash and dry it at a high temperature; inspect body carefully and remove attached ticks with tweezers, grasping the tick as close to the skin surface as possible and pulling straight back with a slow steady force; avoid crushing the tick's body.
Preventive antibiotic treatment with erythromycin or doxycycline to prevent Lyme disease after a known tick bite may be warranted.



1 comment:
Exceptionally very informative article. Great.
Post a Comment